Introduction: What is Parkinson’s Disease?
Parkinson’s disease (PD) is a degenerative neurological disease that is predominantly diagnosed in people over the age of 60. It typically begins with impairments in fine muscle coordination and can progress to include cognitive issues and dementia as well.
The Role of Lewy Bodies and Alpha-Synuclein
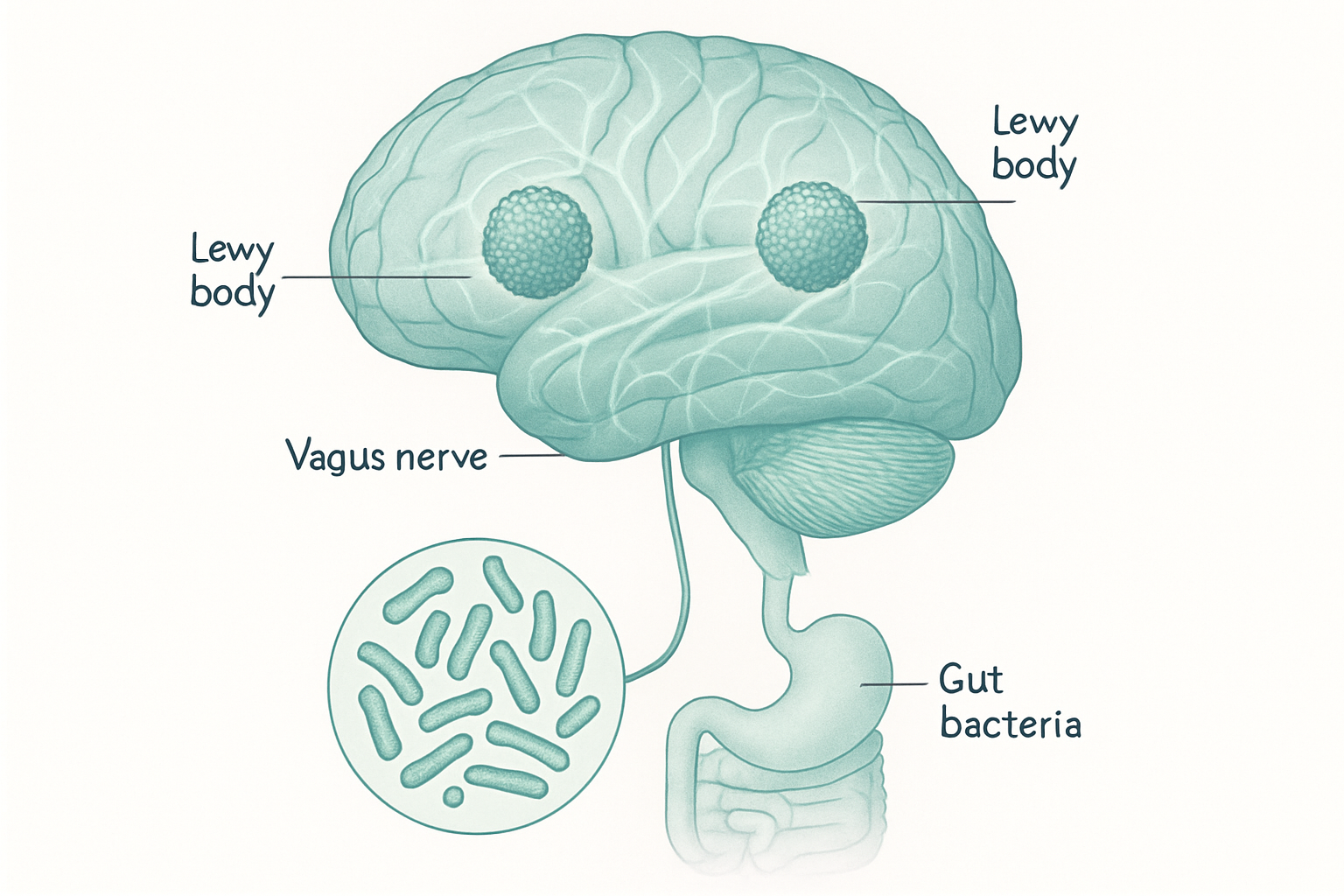
It has been known since the early 1900s that protein clumps in the brain tissue of people with PD, called “Lewy bodies” after Dr. Friedrich H. Lewy, are a very common finding. These clumps are made of a protein called alpha-synuclein, or a-syn. The a-syn protein has a “normal” configuration, but it can also be coaxed into misfolding. It is when misfolded a-syn starts accumulating into Lewy bodies in the brain that the neurological problems begin.
The Ongoing Mystery
While the association between the finding of Lewy bodies in the brain and the diagnosis of PD has been exceedingly strong for over a century now, the role that the Lewy bodies play in the development of the motor and cognitive symptoms of PD have remained a mystery to this day. No clear hypothesis has been put forth to explain the cause of a-syn misfolding, how and why they accumulate in the brain, and what their role is (cause or consequence) in the development and progression of PD.
New Research and Emerging Hypotheses
Way back in my April newsletter I briefly outlined these ideas around Parkinson’s with reference to what was at that time an unpublished article I was co-author on, an article titled Mitochondrial Dysfunction in Parkinson’s Disease: Is Impaired Deuterium Depleted Nutrient Supply by Gut Microbes a Primary Factor? It was, a few months after that, published in the peer-reviewed journal BIOCELL in June 2025.
Recognition and Impact
In less than three months since it was published online it has had over 900 views and 300 downloads. More recently we were contacted by the journal editor and asked to create an image for the cover of the hard-copy edition of the journal because the article is to be the featured article when it comes out at the end of this month.
I think this is all very encouraging. It strongly suggests that the idea of the gut playing a central role in the development of a prominent neurodegenerative disease has gained mainstream credibility.
A Model of Gut-Brain Connection in PD
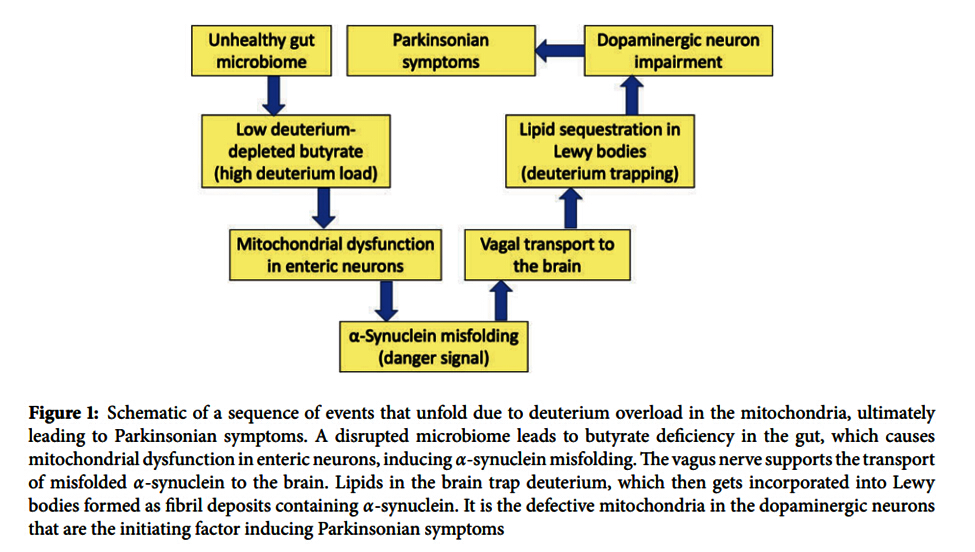
Through the course of peer review the content was improved and images refined. We map out our hypothesis about how all these PD-associated events are tied together, and wouldn’t you know it? It all starts in the unhealthy gut and the deuterium dysregulation that causes. The paper is pretty technical in many areas, but Figure 1 and its caption offers a schematic overview.
https://www.techscience.com/biocell/online
How the Model Works
Start with the box in the upper left corner, “Unhealthy gut microbiome.” For every blue arrow simply read it as “this leads to…” and follow the boxes counter-clockwise back up to the top, “Parkinsonian symptoms.” Note that “enteric neurons” are neurons located in the gut that are physically connected to the vagus nerve, which like a ski lift can pick up misfolded a-syn proteins in the gut, transport them to the specific area in the brain impacted by PD, and drop them off.
Recasting the Disease Process
What I like about this model is that it recasts PD development as the end result of a series of adaptive events (a-syn misfolding and ultimately its accumulation in the brain). Those misfolded a-syn – which originate in the gut, not the brain – are sending a “danger signal” to the brain about the deuterium excess caused by the unhealthy gut microbiome. Even the accumulation of Lewy bodies, commonly understood as a key pathological feature of PD, are here understood to be part of the cellular attempt to “mop up” excess deuterium.
Implications for Chronic Disease Research
New ideas are desperately needed when it comes to understanding the underlying causes of chronic diseases and degenerative diseases. Those new ideas can then lead to new therapeutic approaches. Work on this and other papers related to dysbiosis, as well as to specific nutrient metabolism and biochemistry and its relationship with deuterium regulation in the body, has inspired me to develop a set of unique approaches to not only PD but a wide range of other chronic diseases.
The Spike Protein Connection
As a footnote to this topic, as early as May 2021 Stephanie and I published a peer-reviewed paper suggesting that exposure to the spike protein – whether through infection or mRNA injection – could lead to an increase in PD and other neurological diseases. In fact that increase has already been acknowledged. In 2023 we followed that up with an even more detailed review of how exposure to the mRNA-associated spike protein could provoke an increase in the diagnosis of neurological diseases such as PD and others.
Next Steps and Consultation
If you or someone you know is struggling with any type of progressive neurological disease – Parkinson’s, MS, ALS, Lewy body dementia, or others – we should have a conversation. Treatment strategies have to include assessment of toxic exposures, potential high ongoing spike protein production, dysbiosis and deuterium management, mitochondrial health, and other factors. Schedule a consultation by visiting https://gregnigh.com/schedule, calling 503-719-4806, or emailing drnigh_info@gregnigh.com.